Growing vs. Printing
Twelve years ago, Wake Forest University’s Institute for Regenerative Medicine, based in Winston-Salem, N.C., was the first group in the world to successfully implant a lab-grown bladder in a human. The same group announced in 2011 that it had grown a miniature liver, one inch in diameter, that functions, at least in the lab, as a human liver does.
So if organs can simply be grown in a lab, what’s the fuss about 3D printing? Why not just get some cells in a Petri dish and pour in the cellular Miracle Grow?
Well, for perspective, the first kidney transplant from a living donor happened a mere 59 years ago, with several unsuccessful attempts preceding it. Growing a complex organ from stem cells and then making it function normally when hooked up to the human body will take time to get right. As the process is perfected, it will need to become continuously faster and more streamlined, because organ-transplant patients’ time is limited. As Wake Forest’s website puts it, “One challenge is to learn to grow billions of liver cells at one time in order to engineer livers large enough for patients.” This is where bioprinting comes in.
Atala, a researcher at the forefront of tissue-engineering technology, explains the painstaking process of the 2001 bladder breakthrough. “The bladder scaffold was fashioned by hand and the cells were applied by hand with a pipette,” he says. “With 3D printing, our goal is to make this process more precise. The scaffold would be printed using data from a patient’s medical scans, and the computer controls the placement of cells. This allows for the exact placement of multiple cell types.”
In other words, 3D printing makes an exact replica of a patient’s own organ using his or her own cells. It does this fast, with no breaks, and with precise execution—like an assembly line for organs.
Drugs & Surgery
As the only publicly traded bioprinting company, San DiegoÐbased Organovo has been making the most headlines in the industry. In April, Organovo announced it had printed a 1mm-thick functioning human liver, which had lived for almost a week. “It grew to about twice as thick as we would have expected,” says spokesman Mike Renard. By printing cells that grew into blood vessels, in addition to ones that make the liver function, “it allowed nutrients to go deeper in than would normally be the case,” says Renard.
Though this is still far away from being implantable in a human, it’s a big step in another facet of bioprinting: drug research.
Organovo’s focus right now is making living tissue for use in pharmaceutical research, specifically cancer drugs. Only about one in 5,000 drugs currently in development will make it to market, with an average cost of $1.2 billion per product and 12 years in development. If drug companies were able to test prototypes on specific, living human tissue, time and money needed to produce effective pharmaceuticals would be reduced significantly. “Many drugs fail only after they get into humans,” says Renard. The ability to work on living, human tissue “helps make good decisions about safety and efficacy early in the process.”
TeVido BioDevices, in Austin, Texas, is focused on another area of tissue structures: reconstructive surgery. Led by Dr. Thomas Boland, University of Texas in El Paso faculty member and one of the founding fathers of bioprinting technology, the company is hoping its work on breast tissue will pay off.
Recovery from lumpectomy or mastectomy surgery is often a painful process, physically and emotionally. As far as reconstructive surgery, “right now, there’s really no good option,” says Scott Collins, TeVido’s vice president of research and development. The best scenario may include a tissue graft from a patient’s belly, but that doesn’t allow nipple or areola reconstruction, and it doesn’t react or feel the same. TeVido is working on a process in which living tissue from a patient’s own cells could be printed to exact size and shape specifications within an hour, taking on the body’s natural functions after implantation. “The real work is being done by the cells,” says Collins. “We just have to put them in the right environment so they do what we want them to do.”
This is good news for breast cancer patients and those with the risk-inherent BRCA mutation, which was brought to the wider public eye when actress Angelina Jolie chose to have a preventative double mastectomy after discovering she had an 87 percent chance of developing breast cancer. It’s also good news for plastic surgeons: what can be done to replace what’s been removed can also be done to add to what’s perceived to be lacking.
TeVido was awarded a $150,000 federal grant from Small Business Innovation Research this year. It reads, “The results of this research will help the field move towards larger, clinically relevant tissues and potentially whole organs. The commercial impacts of this research will be the availability of an autologous option for women in the lucrative $10 billion market for breast augmentation.”
Burn Victims Rejoice
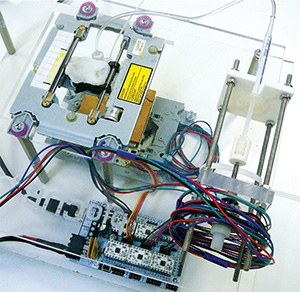
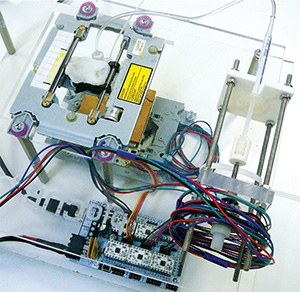
The team at Wake Forest is also working on printing skin cells directly onto burn victims with severe injuries who otherwise might need skin grafts culled from their back or buttocks. Kyle Binder, a lab scientist at Wake Forest’s Armed Forces Institute of Regenerative Medicine, explains in a video from Lab TV that the process involves “taking a normal desktop ink-jet printer, and you load the cartridge with cells instead of ink, and just using the normal method . . . you can print out human tissue instead of ink.”
The video shows a stunningly lo-fi version of a bioprinter, literally a home desktop printer with the cover removed, its guts modified to save lives instead of to print tax forms. Burns can account for 10 to 30 percent of all casualties on a battlefield, hence the Army’s interest in the technology, but it will also be able useful for treating burn victims on-site, like firefighters or other emergency personnel.
How it works is pretty simple: a camera scans the wound, making a 3D map with lasers, and a computer sorts out where and what to print onto the skin. The wound is filled, and—presto—the cells grow into new skin. Though this already sounds futuristic, the video of this demonstration is three years old. Since then, the Wake Forest team has updated the machine and has had success working on mice, closing a wound in two weeks that normally takes five weeks to heal. Most human victims of burns that severe will die within two weeks due to infection.
Life on Mars
Sculptor and NYU art professor Robert Michael Smith is also involved in advancing bioprinting technology, but not for obvious reasons. “I want to be the first sculptor with a sculpture on Mars, except that it will be a created living form,” says the artist, who counts Montgomery High School and Santa Rosa Junior College among his alma maters. Smith, whose work was featured at Healdsburg’s Hammerfriar Gallery earlier this year, has already designed and printed 3D sculptures for this purpose, even integrating living cells using a bioprinter like the one at Wake Forest. His hope is to use the technology with his own DNA to perform tests on living, human cells during space missions to Mars. This would, in a way, make him the first human being to travel to Mars.
Smith reached out to Dr. Atala, who was receptive to the idea. “When you are exploring new venues in science, you always have to break through dogma,” says Atala in a discussion with Smith on YouTube. Atala says the idea is possible with current technology, though it would be an “expensive proposition.”
Smith says his vision includes a version of Wake Forest’s bioprinter for further experiments on the Red Planet. Like testing new treatments in drug research, Smith sees the possibility of evaluating the effects of intense, prolonged space travel on a cellular level using living tissue systems created with a bioprinter. “Why should any sentient creature be sacrificed when we can be creating physical simulators?” he asks, citing reports of people already signed up for a one-way “suicide mission” to study the planet’s potential for colonization. “Human beings are going to do whatever human beings are going to do,” says Smith. “Whether I’m involved or not, this is going to move forward.”
Laws & Regulations
Due to the United States’ regulatory system and insurance billing codes, Collins says TeVido’s breast-tissue research is likely to be implemented in the cosmetic market before the medical industry is able to take full advantage of it. Collins estimates that cosmetic procedures using this technology could be taking place within 10 years, while the FDA is looking at clinical trials and making up its mind on using the technology in medical applications. “Medical technology is getting a lot more complex very quickly, and we’re kind of overloading the system,” Collins says.
Waiting for the tortoise-like government-approval process to finalize means that, in the meantime, there’s no money coming in. One way to combat this is to license the technology for use in other countries. “That is not ideal,” says Collins, “but it’s the way many companies work in this space right now.”
Just a few months ago, Hangzhou Dianzi University in China announced it had made a 3D tissue printer that successfully printed functional miniature liver samples and ear cartilage. An orthopedic surgeon in Southern California is working on a technique involving printing cartilage from a patient’s own cells that might eventually replace dangerous and limiting spinal-fusion surgery. And perhaps most promising, a company in New England recently engineered a small kidney that produced a urine-like substance when implanted in a steer. The technology is here. It’s just in the “making sure it’s safe” phase.
Once the technology is shown to be safe, which is on track to happen in our lifetime, new organs will appear out of thin air more often than from another human. The “organ donor” section on a drivers’ license application could become a whimsical nod to the past. The waiting list for transplants could be eliminated.
In the world of 3D bioprinting, survival could be a point and click away.


